Research | Departments
Research
Departments
Research | Departments
Research
Departments
Dr. Chou’ research topics include lung pathology, molecular pathology of lung cancer, and precision medicine of cancer. As a practicing pulmonary pathologist, the projects Dr. Chou has been working on in recent 20 years focus on the molecular mechanisms of tumor metastasis and prediction and prognostication biomarkers of lung cancer. Through grants sponsored by the government as well as the industries, Dr. Chou has accomplished several seminal scientific discoveries, which are well illustrated in his more than 150 articles published in international SCI journals. With the continuous efforts on the study of lung cancer, Dr. Chou’s laboratory is to apply state-of-the-art molecular pathology and precision medicine technologies on human specimens to search for biomarkers and therapy targets of tumor occurrence, progression, recurrence and drug resistance in lung cancer.
Email | tehying@tmu.edu.tw
Profile | Academic Hub/Pure Experts
Professor (M.D., Ph.D.)
Pulmonary Pathology, Molecular Pathology of Lung Cancer Metastasis, Invasion and Metastasis of Lung Cancer, Cancer Glycobiology, Precision Medicine
Laboratory of Thoracic Precision Oncology
Prof./Dr. Chou was born in 1959 and received an M.D. degree from the National Yang-Ming Medical College, Taipei, Taiwan in 1984. After the anatomical pathology residency training at the Taipei Veterans General Hospital, he went to the Johns Hopkins University School of Medicine and received a Ph.D. degree in Biochemistry in 1995.
In his thesis work advised by Professor Gerald Hart and Professor Chi Dang, Dr. Chou provided the evidence of O-GlcNAc glycosylation of the oncoprotein c-Myc. From 1999 to 2001, he completed an anatomic pathology residency at the Washington University Medical Center/Barnes-Jewish Hospital and, from 2001 to 2002, a Calendar Binford Clinical Fellowship in Pulmonary Pathology with Professor William D. Travis in the Department of Pulmonary and Mediastinal Pathology, Armed Forces Institute of Pathology.
After returning to his hometown in 2002, Dr. Chou resumed an attending pathologist position at the Taipei Veterans General Hospital. From 2014 to 2017, Dr. Chou was President of the Taiwan Society of Pathology as well as the Taiwan Division of International Academy of Pathology. Since 2014, Dr. Chou has been a member of the Pathology Committee of International Association for the Study of Lung Cancer (IASLC).
In 2016, Dr. Chou received a master degree in Business Administration from the National Taiwan University, Taipei, Taiwan. Dr. Chou is currently Professor of the Graduate Institute of Clinical Medicine, Taipei Medical University and Vice Superintendent for Research and Development, Taipei Medical University Hospital.
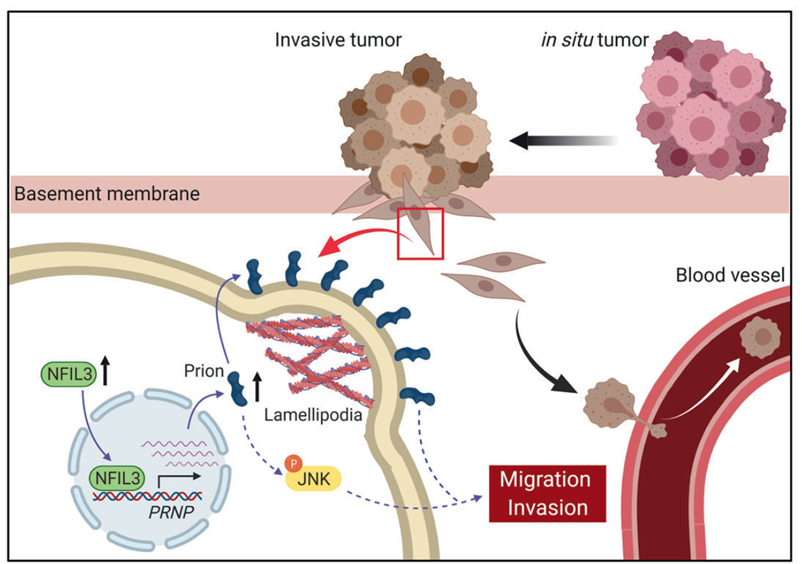
His major scientific achievements include the identification of a regulatory hub of developmental/stemness signaling and invadopodia that drives cancer stemness and progression, which may hold promises for development into novel CSC-targeted therapies. He co-identified a cell-intrinsic and chromatin-mediated cellular “death checkpoint” whereby most malignant tumors resist cytotoxic stress; the targeting of which yields an exciting opportunity for sensitizing malignant tumors to chemotherapy and immunotherapy.
Ph.D. (Postdoctoral Fellow)
MD (PhD Student)
MD (PhD Student)
MS (PhD Student)
MS (PhD Student)
MD (Research Assistant)
Yang CY, Yeh YC, Wang LC, Lin YY, Lin SY, Wang SY, Chu PY, Liu ZY, Su YC, Ho HL*, Chou TY*.
Genomic profiling with large-scale next-generation sequencing panels distinguishes separate primary lung adenocarcinomas from intrapulmonary metastases.
Modern Pathology. 36 (2023) 100047
Abstract
The distinction between different separate primary lung cancers (SPLCs) and intrapulmonary metastases (IPMs) is a challenging but clinically significant issue. Histopathology-based classification is the current practice; however, it is subjective and affected by interobserver variability. Recently, next-generation sequencing (NGS) panels have been used in lung cancer diagnostics. This study aimed to investigate the value of large-scale NGS panels for distinguishing between SPLCs and IPMs. A total of 32 patients with 69 lung adenocarcinomas were included. Comprehensive histopathologic assessments of multiple pulmonary adenocarcinomas were performed independently by 3 pathologists. The consensus of histopathologic classification was determined by a majority vote. Genomic analysis was performed using an amplicon-based large-scale NGS panel, targeting single-nucleotide variants and short insertions and deletions in 409 genes. Tumor pairs were classified as SPLCs or IPMs according to a predefined molecular classification algorithm. Using NGS and our molecular classification algorithm, 97.6% of the tumor pairs can be unambiguously classified as SPLCs or IPMs. The molecular classification was predictive of postoperative clinical outcomes in terms of overall survival (P = .015) and recurrence-free interval (P = .0012). There was a moderate interobserver agreement regarding histopathologic classification (κ = 0.524 at the tumor pair level). The concordance between histopathologic and molecular classification was 100% in cases where pathologists reached a complete agreement but only 53.3% where they did not. This study showed that large-scale NGS panels are a powerful modality that can help distinguish SPLCs from IPMs in patients with multiple lung adenocarcinomas and objectively provide accurate risk stratification.
Lin YY, Wang LC, Hsieh YH, Hung YL, Chen YA, Lin YC, Lin YY, Chou TY*.
Computer-assisted threedimensional quantitation of programmed death-ligand 1 in non-small cell lung cancer using tissue clearing technology.
Journal of Translational Medicine. (2022) Mar 16;20(1):131
Abstract
Immune checkpoint blockade therapy has revolutionized non-small cell lung cancer treatment. However, not all patients respond to this therapy. Assessing the tumor expression of immune checkpoint molecules, including programmed death-ligand 1 (PD-L1), is the current standard in predicting treatment response. However, the correlation between PD-L1 expression and anti-PD-1/PD-L1 treatment response is not perfect. This is partly caused by tumor heterogeneity and the common practice of assessing PD-L1 expression based on limited biopsy material. To overcome this problem, we developed a novel method that can make formalin-fixed, paraffin-embedded tissue translucent, allowing three-dimensional (3D) imaging. Our protocol can process tissues up to 150 μm in thickness, allowing anti-PD-L1 staining of the entire tissue and producing high resolution 3D images. Compared to a traditional 4 μm section, our 3D image provides 30 times more coverage of the specimen, assessing PD-L1 expression of approximately 10 times more cells. We further developed a computer-assisted PD-L1 quantitation method to analyze these images, and we found marked variation of PD-L1 expression in 3D. In 5 of 33 needle-biopsy-sized specimens (15.2%), the PD-L1 tumor proportion score (TPS) varied by greater than 10% at different depth levels. In 14 cases (42.4%), the TPS at different depth levels fell into different categories (<1%, 1–49%, or≧50%), which can potentially influence treatment decisions. Importantly, our technology permits recovery of the processed tissue for subsequent analysis, including histology examination, immunohistochemistry, and mutation analysis. In conclusion, our novel method has the potential to increase the accuracy of tumor PD-L1 expression assessment and enable precise deployment of cancer immunotherapy.
Lin CH, Liao CC, Wang SY, Peng CY, Yeh YC, Chen MY*, Chou TY*.
Comparative O-GlcNAc Proteomic Analysis Reveals a Role of O-GlcNAcylated SAM68 in Lung Cancer Aggressiveness.
Cancers (Basel). (2022) Jan 4;14(1):243
Abstract
O-GlcNAcylation is a reversible and dynamic post-translational protein modification catalyzed by O-GlcNAc transferase (OGT). Despite the reported association of O-GlcNAcylation with cancer metastasis, the O-GlcNAc proteome profile for cancer aggressiveness remains largely uncharacterized. Here, we report our comparative O-GlcNAc proteome profiling of two differentially invasive lung adenocarcinoma cell lines, which identified 158 down-regulated and 106 up-regulated candidates in highly invasive cells. Among these differential proteins, a nuclear RNA-binding protein, SAM68 (SRC associated in mitosis of 68 kDa), was further investigated. Results showed that SAM68 is O-GlcNAcylated and may interact with OGT in the nucleus. Eleven O-GlcNAcylation sites were identified, and data from mutant analysis suggested that multiple serine residues in the N-terminal region are important for O-GlcNAcylation and the function of SAM68 in modulating cancer cell migration and invasion. Analysis of clinical specimens found that high SAM68 expression was associated with late cancer stages, and patients with high-OGT/high-SAM68 expression in their tumors had poorer overall survival compared to those with low-OGT/low-SAM68 expression. Our study revealed an invasiveness-associated O-GlcNAc proteome profile and connected O-GlcNAcylated SAM68 to lung cancer aggressiveness.
Lin YY, Wang YC, Yeh DW, Hung CY, Yeh YC, Ho HL, Mon HC, Chen MY, Wu YC, Chou TY*.
Gene Expression Profile in Primary Tumor Is Associated with Brain-Tropism of Metastasis from Lung Adenocarcinoma.
International Journal of Molecular Science. (2021) Dec 13;22(24):13374
Abstract
Lung adenocarcinoma has a strong propensity to metastasize to the brain. The brain metastases are difficult to treat and can cause significant morbidity and mortality. Identifying patients with increased risk of developing brain metastasis can assist medical decision-making, facilitating a closer surveillance or justifying a preventive treatment. We analyzed 27 lung adenocarcinoma patients who received a primary lung tumor resection and developed metastases within 5 years after the surgery. Among these patients, 16 developed brain metastases and 11 developed non-brain metastases only. We performed targeted DNA sequencing, RNA sequencing and immunohistochemistry to characterize the difference between the primary tumors. We also compared our findings to the published data of brain-tropic and non-brain-tropic lung adenocarcinoma cell lines. The results demonstrated that the targeted tumor DNA sequencing did not reveal a significant difference between the groups, but the RNA sequencing identified 390 differentially expressed genes. A gene expression signature including CDKN2A could identify 100% of brain-metastasizing tumors with a 91% specificity. However, when compared to the differentially expressed genes between brain-tropic and non-brain-tropic lung cancer cell lines, a different set of genes was shared between the patient data and the cell line data, which include many genes implicated in the cancer-glia/neuron interaction. Our findings indicate that it is possible to identify lung adenocarcinoma patients at the highest risk for brain metastasis by analyzing the primary tumor. Further investigation is required to elucidate the mechanism behind these associations and to identify potential treatment targets.
Lin CH, Liao CC, Chen MY, Chou TY*.
Feedback Regulation of O-GlcNAc Transferase through Translation Control to Maintain Intracellular O-GlcNAc Homeostasis.
International Journal of Molecular Science. (2021) Mar 27;22(7):3463
Abstract
Protein O-GlcNAcylation is a dynamic post-translational modification involving the attachment of N-acetylglucosamine (GlcNAc) to the hydroxyl groups of Ser/Thr residues on numer-ous nucleocytoplasmic proteins. Two enzymes are responsible for O-GlcNAc cycling on substrate proteins: O-GlcNAc transferase (OGT) catalyzes the addition while O-GlcNAcase (OGA) helps the removal of GlcNAc. O-GlcNAcylation modifies protein functions; therefore, dysregulation of O-GlcNAcylation affects cell physiology and contributes to pathogenesis. To maintain homeostasis of cellular O-GlcNAcylation, there exists feedback regulation of OGT and OGA expression responding to fluctuations of O-GlcNAc levels; yet, little is known about the molecular mechanisms involved. In this study, we investigated the O-GlcNAc-feedback regulation of OGT and OGA expression in lung cancer cells. Results suggest that, upon alterations in O-GlcNAcylation, the regulation of OGA expression occurs at the mRNA level and likely involves epigenetic mechanisms, while modulation of OGT expression is through translation control. Further analyses revealed that the eukaryotic translation initiation factor 4E-binding protein 1 (4E-BP1) contributes to the downregulation of OGT induced by hyper-O-GlcNAcylation; the S5A/S6A O-GlcNAcylation-site mutant of 4E-BP1 cannot support this regulation, suggesting an important role of O-GlcNAcylation. The results provide additional insight into the molecular mechanisms through which cells may fine-tune intracellular O-GlcNAc levels to maintain homeostasis.







 Total Users : 362201
Total Users : 362201
 Tsu-Yi Chao
Tsu-Yi Chao 