Research | Departments
Research
Departments
Research | Departments
Research
Departments
Cancer metastasis and treatment resistance are the two main causes of patient mortality, whereas the underlying cellular and molecular mechanisms are still far from clear. Notwithstanding many decades of basic and clinical research, the therapeutic outcome of cancer patients remains less than satisfactory. The research at the Laboratory of Advanced Molecular Therapeutics (AMT Lab) is aimed at identifying novel and critical regulators of cancer metastasis and treatment resistance that may have important diagnostic and therapeutic implications. Our group uses unique and integrative approaches combining genetics, proteomics, bioinformatics, and tissue engineering principles to study cancer metastasis and its heterogeneity. Our work in these themes has led to the identification of key mediators and novel mechanisms of cancer stemness and metastasis, which provides new insights into cancer aggressiveness. Another line of our research is focused on the role of chemotherapy-treated stroma in tumor progression and therapeutic failure. We have uncovered a paradoxically oncogenic role of chemotherapy-treated stromal cells in pancreatic cancer and breast cancer, and have delineated the underlying signaling pathways and molecular mechanisms. Targeting the therapy-induced stromal-epithelial signaling may be a new avenue for improving the therapeutic outcome of cancer patients. Overall, the main thrusts of the research at the AMT Lab include the following major areas:
Increasing evidence suggests that cancer stem cells (CSCs) are the major driving force of cancer dissemination and distant metastasis. It is plausible that therapies targeting the subpopulation of CSCs with high metastasis potentials, the so-called “metastatic CSCs”, may yield potential therapeutic opportunities for metastatic cancer and hold considerable promises for improving patients’ outcomes.
The Wnt pathway plays a crucial role in cancer stemness. Activation of Wnt signaling in CSCs at the distant metastasis sites dictates the successful colonization of the infiltrated cancer cells. The AMT Lab led by Dr. Tsai has identified a novel oncoprotein, ASPM (abnormal spindle-like microcephaly associated), which maintains the oncogenic and invasive potential of CSCs in a wide variety of cancers, including pancreatic, gastric, prostate, lung, and liver cancers. We show that isoform 1 of ASPM specifically augments Wnt signaling by positively regulating Dishevelled proteins in various cancers (Gastroenterology 2013; Oncogene 2018; Journal of Pathology 2019; Cancer Research 2023). Our subsequent works further unraveled the role of ASPM-i1 as a regulatory hub of development-associated signaling pathways, including Wnt, Hedgehog, Notch, and Hippo pathways, in cancer cells and CSCs (Cancer Research 2023). We are currently investigating the role of ASPM-i1 in other cancer biology, such as invadopodia biogenesis, and exploiting its potential utility as a pathway- and stemness-informed prognostic biomarker and therapeutic target in advanced and aggressive cancers.
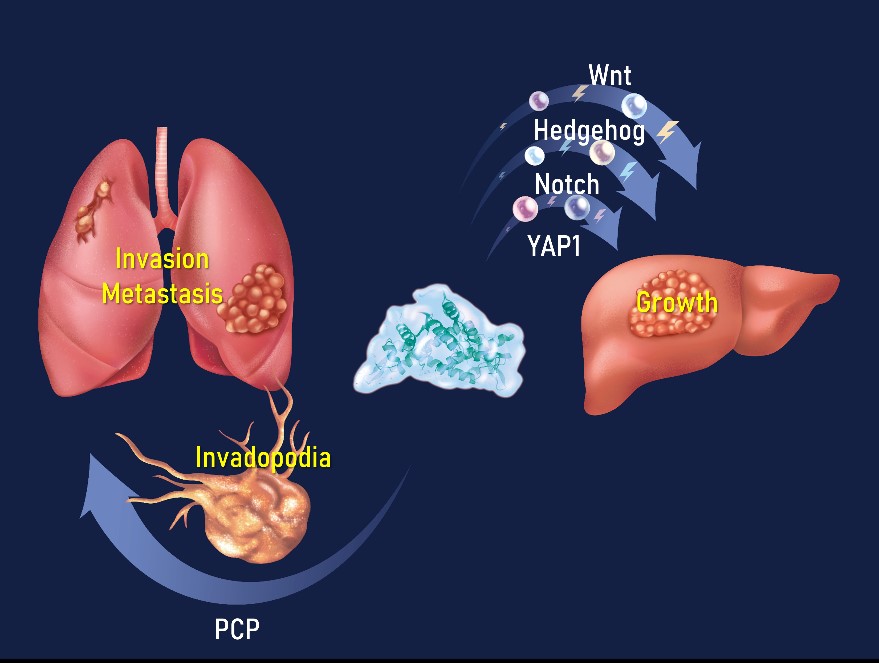
Figure 1. ASPM as the regulatory hub of cancer growth, invasion, and metastasis (AMT Lab 2023).
Resistance to anti-tumor treatment contributes to patient mortality. Functional proteomic screening of chemotherapy-treated breast cancer patient-derived organoids (PDOs) identified nuclear co-repressor-2 (NCOR2) histone deacetylase as an inhibitor of cytotoxic stress response and anti-tumor immunity (Nature Cancer 2022). High NCOR2 in the tumors of breast cancer patients predicted chemotherapy refractoriness, tumor recurrence, and poor prognosis. Molecular studies revealed that the NCOR2/HADC3 “Death Checkpoint” inhibits anti-tumor treatment by repressing IRF1-dependent gene expression and interferon (IFN) signaling. Reducing NCOR2 or impeding its epigenetic activity by modifying its interaction with HDAC3 enhanced chemotherapy responsiveness and restored anti-tumor immunity.
We developed a “Decoy of NCOR2” gene therapy, which potentiated chemo-, and immune checkpoint therapy by dismantling the NCOR2 Death Checkpoint, thus permitting transcription of IRF1-regulated pro-apoptosis and inflammatory genes in response to therapies. The discovery underscores the power of using PDOs for anti-tumor drug studies. Targeting stress and inflammatory-repressor complexes such as the NCOR2/HDAC3 Death Checkpoint could overcome treatment resistance and improve cancer patient outcomes (video abstract featured in Research Square: https://www.researchsquare.com/article/rs-3462346/v1).


Email | tsaik@tmu.edu.tw
Profile | Academic Hub/Pure Experts
Professor (M.D., Ph.D.)
Cell and Molecular Biology, Cancer Biology, Cancer Stem Cells, Cancer Molecular Medicine, Pancreatic Cancer, Breast Cancer, Cancer Treatment Resistance
Laboratory of Advanced Molecular Therapeutics (AMT Lab)
Dr. Tsai is a rigorously trained physician-scientist focusing on basic and translational cancer research with a career goal aiming at developing breakthrough therapeutics targeting cancer aggressiveness and treatment refractoriness. Dr. Tsai graduated with an M.D. from Taipei Medical University (Taiwan) in 1993, and completed his clinical training in internal medicine, gastroenterology, and GI oncology. Dr. Tsai then earned his Ph.D. in Biological Sciences – Genetics and Complex Diseases from Graduate School of Arts and Sciences, Harvard University (MA, USA) in 2005. During his thesis work, Dr. Tsai established novel 3D coculture models to interrogate stress-induced stromal-epithelial interactions. In 2007, he conducted postdoctoral research at the University of Pennsylvania (PA, USA) and the University of California San Francisco (CA, USA) and spearheaded the study of novel tissue-architecture-related mechanisms of multi-drug resistance in cancer. Following his postdoc research, Dr. Tsai joined the National Institute of Cancer Research in National Health Research Institutes (NHRIs) as an Investigator, and then became the Director and Professor of Graduate Institute of Clinical Medicine at Taipei Medical University. Dr. Tsai is the recipient of many awards, including Harvard Presidential Scholar, USA, Outstanding Research Award, Taiwan, Kobayashi’s Foundation Award, Japan, and Young Scientists Research Achievement Award of NHRIs, Taiwan. He is the first or corresponding author of more than 30 research papers in top-notch biomedical journals such as Nature Cancer, Gastroenterology, J Exp Med, J Am Coll Cardiol, Gut, Cancer Res, etc, and he also served as the PI in several GI cancer-related clinical trials. His major scientific achievements include the identification of a regulatory hub of developmental/stemness signaling and invadopodia that drives cancer stemness and progression, which may hold promises for development into novel CSC-targeted therapies. He co-identified a cell-intrinsic and chromatin-mediated cellular “death checkpoint” whereby most malignant tumors resist cytotoxic stress; the targeting of which yields an exciting opportunity for sensitizing malignant tumors to chemotherapy and immunotherapy.
Dr. Tsai graduated with an M.D. from Taipei Medical University (Taiwan) in 1993, and completed his clinical training in internal medicine, gastroenterology, and GI oncology. Dr. Tsai then earned his Ph.D. in Biological Sciences – Genetics and Complex Diseases from Graduate School of Arts and Sciences, Harvard University (MA, USA) in 2005. During his thesis work, Dr. Tsai established novel 3D coculture models to interrogate stress-induced stromal-epithelial interactions.
In 2007, he conducted postdoctoral research at the University of Pennsylvania (PA, USA) and the University of California San Francisco (CA, USA) and spearheaded the study of novel tissue-architecture-related mechanisms of multi-drug resistance in cancer. Following his postdoc research, Dr. Tsai joined the National Institute of Cancer Research in National Health Research Institutes (NHRIs) as an Investigator, and then became the Director and Professor of Graduate Institute of Clinical Medicine at Taipei Medical University.
Dr. Tsai is the recipient of many awards, including Harvard Presidential Scholar, USA, Outstanding Research Award, Taiwan, Kobayashi’s Foundation Award, Japan, and Young Scientists Research Achievement Award of NHRIs, Taiwan. He is the first or corresponding author of more than 30 research papers in top-notch biomedical journals such as Nature Cancer, Gastroenterology, J Exp Med, J Am Coll Cardiol, Gut, Cancer Res, etc, and he also served as the PI in several GI cancer-related clinical trials.
His major scientific achievements include the identification of a regulatory hub of developmental/stemness signaling and invadopodia that drives cancer stemness and progression, which may hold promises for development into novel CSC-targeted therapies. He co-identified a cell-intrinsic and chromatin-mediated cellular “death checkpoint” whereby most malignant tumors resist cytotoxic stress; the targeting of which yields an exciting opportunity for sensitizing malignant tumors to chemotherapy and immunotherapy.
Ph.D. (postdoctoral researcher)
Ph.D. (postdoctoral researcher)
M.S. (lab manager)
Cheng LH, Hsu CC, Liao WY, Yang PM, Liao TY, Chan TS, Tsai KK.
ASPM activates Hedgehog and Wnt signaling to promote small cell lung cancer stemness and progression.
Cancer Research 2023;83:830-844 (IF=13.312; corresponding author).
Abstract
Small cell lung cancer (SCLC) is among the most aggressive and lethal human malignancies. Most patients with SCLC who initially respond to chemotherapy develop disease relapse. Therefore, there is a pressing need to identify novel driver mechanisms of SCLC progression to unlock treatment strategies to improve patient prognosis. SCLC cells comprise subsets of cells possessing progenitor or stem cell properties, while the underlying regulatory pathways remain elusive. Here, we identified the isoform 1 of the neurogenesis-associated protein ASPM (ASPM-I1) as a prominently upregulated stemness-associated gene during the self-renewal of SCLC cells. The expression of ASPM-I1 was found to be upregulated in SCLC cells and tissues, correlated with poor patient prognosis, and indispensable for SCLC stemness and tumorigenesis. A reporter array screening identified multiple developmental signaling pathways, including Hedgehog (Hh) and Wnt pathways, whose activity in SCLC cells depended upon ASPM-I1 expression. Mechanistically, ASPM-I1 stabilized the Hh transcriptional factor GLI1 at the protein level through a unique exon-18-encoded region by competing with the E3 ligases β-TrCP and CUL3. In parallel, ASPM-I1 sustains the transcription of the Hh pathway transmembrane regulator SMO through the Wnt-DVL3-β-catenin signaling axis. Functional studies verified that the ASPM-I1-regulated Hh and Wnt activities significantly contributed to SCLC aggressiveness in vivo. Consistently, the expression of ASPM-I1 positively correlated with GLI1 and stemness markers in SCLC tissues. This study illuminates an ASPM-I1-mediated regulatory module that drives tumor stemness and progression in SCLC, providing an exploitable diagnostic and therapeutic target.
Tsai KK, Bae BI, Hsu CC, Cheng LH, Shaked Y.
Oncogenic ASPM is a regulatory hub of developmental and stemness signaling in cancer.
Cancer Research 2023;83:2993-3000 (IF=13.312; first and corresponding author).
Abstract
Despite recent advances in molecularly targeted therapies and immunotherapies, the effective treatment of advanced-stage cancers remains a largely unmet clinical need. Identifying driver mechanisms of cancer aggressiveness can lay the groundwork for the development of breakthrough therapeutic strategies. Assembly factor for spindle microtubules (ASPM) was initially identified as a centrosomal protein that regulates neurogenesis and brain size. Mounting evidence has demonstrated the pleiotropic roles of ASPM in mitosis, cell-cycle progression, and DNA double-strand breaks (DSB) repair. Recently, the exon 18-preserved isoform 1 of ASPM has emerged as a critical regulator of cancer stemness and aggressiveness in various malignant tumor types. Here, we describe the domain compositions of ASPM and its transcript variants and overview their expression patterns and prognostic significance in cancers. A summary is provided of recent progress in the molecular elucidation of ASPM as a regulatory hub of development- and stemness-associated signaling pathways, such as the Wnt, Hedgehog, and Notch pathways, and of DNA DSB repair in cancer cells. The review emphasizes the potential utility of ASPM as a cancer-agnostic and pathway-informed prognostic biomarker and therapeutic target.
Tsai KK, Huang SS, Northey J, Liao WY, Hsu CC, Cheng LH, Werner M, Chuu CP, Chatterjee C, Lakins, JN, Weaver VM*.
Screening of organoids derived from patients with breast cancer implicates the repressor NCOR2 in cytotoxic stress response and anti-tumor immunity.
Nature Cancer 2022;3:734-752 (IF=23.177; first and co-corresponding author).
Abstract
–
Chan TS, Hsu CC, Pai VC, Liao WY, Huang SS, Tan KT, Yen CJ, Hsu SC, Chen WY, Shan YS, Li CR, Lee MT, Jian KY, Chu JM, Lien GS, Weaver VM, Tsai KK.
Metronomic chemotherapy prevents therapy-induced stromal activation and induction of tumor-initiating cells.
Journal of Experimental Medicine 2016;213:2967-2988 (IF=17.579; corresponding author
Abstract
–
Wang WY, Hsu CC, Wang TY, Li CR, Hou YC, Chu JM, Lee CT, Liu MS, Su JJ, Jian KY, Huang SS, Jiang SS, Shan YS, Lin PW, Shen YY, Lee MT, Chan TS, Chang CC, Chen CH, Chang IS, Lee YL, Chen LT, Tsai KK.
A gene expression signature of epithelial tubulogenesis and a role for ASPM in pancreatic tumor progression.
Gastroenterology 2013;145:1110-1120 (IF=33.883; corresponding author).
Abstract
–







 Total Users : 234525
Total Users : 234525
 Chiung-Chi Peng
Chiung-Chi Peng 